
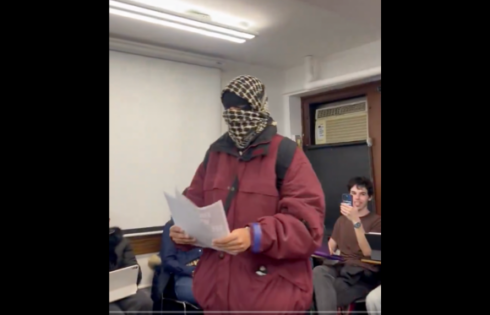
OPINION: Students are expected to comply with a casual indifference usually reserved for having to obtain the correct parking pass
Across the country students at an ever growing number of universities face vaccine mandates for COVID-19.
Nine months ago concerns about such requirements were regarded as belonging to the realm of conspiracy theorists – especially while the vaccines were technically still experimental.
Then Rutgers mandated COVID vaccination for their students. A lot of other private universities followed. Then a lot of public universities did the same as everyone memory-holed the notion that a university couldn’t mandate an experimental drug.
By the end of summer, the exact status of COVID vaccines as having full FDA approval or being authorized for emergency use was treated by more and more schools as a mere technicality.
And now, with the full approval of the Pfizer vaccine, it seems inevitable that a wave of universities yet to issue vaccine mandates will finally do so while those that have allowed personal exemptions will begin revoking them.
Yet, in the mass fit of group-think that led to an environment in which university bureaucrats have become fixated with a Hellerian arithmetic in which COVID cases are calculated as black eyes and vaccinations are counted as feathers in their caps, many important questions get casually dismissed without meaningful discussion or consideration.
Do traditional-aged college students really need to be vaccinated for COVID-19? Should students be concerned about potential side-effects? Does it matter if they have already had and recovered from COVID? And, in some way, don’t these policies constitute a violation of a student’s personal and medical autonomy?
As early as April 2020, when the timeline for the development and distribution of a COVID vaccine remained uncertain, university presidents from around the country, as they attempted to justify a return to in-person learning for that fall, made claims their students were at incredibly low risk from COVID-19.
Mitch Daniels of Purdue described the virus as posing “close to zero lethal threat to them.” Christina Paxson of Brown wrote in a New York Times editorial, “a vast majority of residential college students will experience only mild symptoms if they contract the coronavirus.” And, in the months that followed, these claims were validated time and time again as COVID was shown to be a largely survivable illness, especially for those under 65 and in good health.
Later in the year, when it became apparent we would have a COVID vaccine available at warp-speed, many rejoiced, although circumspect individuals with knowledge of the standard vaccine development process cautioned that exponentially accelerating this process was not without risk.
An article in Toxicology Reports warned that mid- and long-term safety testing would not be possible on this schedule, acknowledging, “Vaccine development, including limited safety testing, has taken an average of 12–15 years” and warning that, “There are many potential adverse health effects that can result from vaccine-induced mechanisms … these effects could emerge in the near-term or the long-term. To require the young people (who are not at risk from the most serious consequences of COVID-19) to take such vaccines with potential serious long-term consequences is unjustifiable.”
Among the “potential adverse health effects” about which the article in Toxicology Reports warned were a number of conditions stemming from autoimmune or enhanced immune responses.
In the short-term, some of these including Guillain-Barré syndrome, Bell’s palsy, myocarditis and pericarditis, have already been reported in individuals shortly after COVID vaccination, as has multisystem inflammatory syndrome, the risk of which appears to increase if one is vaccinated for COVID following COVID infection.
To be clear, such adverse events seem to be rare, at least in the short-term, but, once more, so are COVID deaths among young, healthy individuals. Hence, whether a healthy college student chooses to get vaccinated or not, said college student is making a choice and taking a small risk. Yet, the exact equation for assessing that risk is far from settled and likely varies between individuals.
For a less healthy college student who is perhaps obese, COVID vaccination is probably a sensible precaution. For the average college student, the slight risk of myocarditis or the unknown risk of a more serious autoimmune condition that may develop later might outweigh whatever marginal benefit they would potentially receive from vaccination.
For a student currently living with an autoimmune condition or with family members who have already experienced Guillain-Barré syndrome or Bell’s palsy after having their COVID vaccine, caution may be far more warranted.
An additional variable to be factored into this equation is previous COVID infection, not only because it may put some people at a greater risk of certain side-effects, but because it also appears to confer a level of immunity comparable to, if not better than, that attained through vaccination. This has been demonstrated repeatedly by researchers from such schools as Emory, UCSD, and Washington University School of Medicine. Recently it has also been confirmed through real-world observation in Israel.
In the current academic landscape, however, this complex, personal medical decision has been reduced to a matter of institutional box-checking. Universities that wish to demonstrate they take COVID seriously, and perhaps shield themselves from potential lawsuits or bad PR in the event of an outbreak, mandate vaccination.
Students are expected to comply with a casual indifference usually reserved for having to obtain the correct parking pass. Those who object can perhaps request some form of exemption, but receiving one is far from guaranteed.
Prior COVID infection generally tends not to be deemed a valid excuse to not be vaccinated for COVID. BYU Hawaii even denied a medical exemption to a student with a documented medical history suggesting COVID vaccination to be a meaningful threat to her health.
To avoid having to justify these policies or decisions, many universities simply claim they are just following public health guidance.
Yet, contrary to the implied assumption of these universities, neither the CDC nor FDA nor any one public health official is the ultimate arbiter of scientific truth or medical fact -– especially with regard to an illness that has existed for just under two years.
Furthermore, some of the guidance issued by the authorities to which universities appeal has been truly baffling (e.g. those who recovered from COVID should be vaccinated for COVID).
Even more baffling though is why a generation of young people should be required to relinquish control of a personal medical decision to university bureaucrats more concerned with an arbitrary ratio of black eyes to feathers in their caps than a very real, individual risk-benefit analysis of whether one has more to gain than lose from an often unnecessary medical treatment developed at warp speed.
MORE: Colleges requiring COVID vaccine will not accept acquired immunity as alternative
IMAGE: Studio Romantic
Like The College Fix on Facebook / Follow us on Twitter





Please join the conversation about our stories on Facebook, Twitter, Instagram, Reddit, MeWe, Rumble, Gab, Minds and Gettr.